2026 Guide For Patient Intake Automation: Top 8 AI-Powered Patient Intake Tools
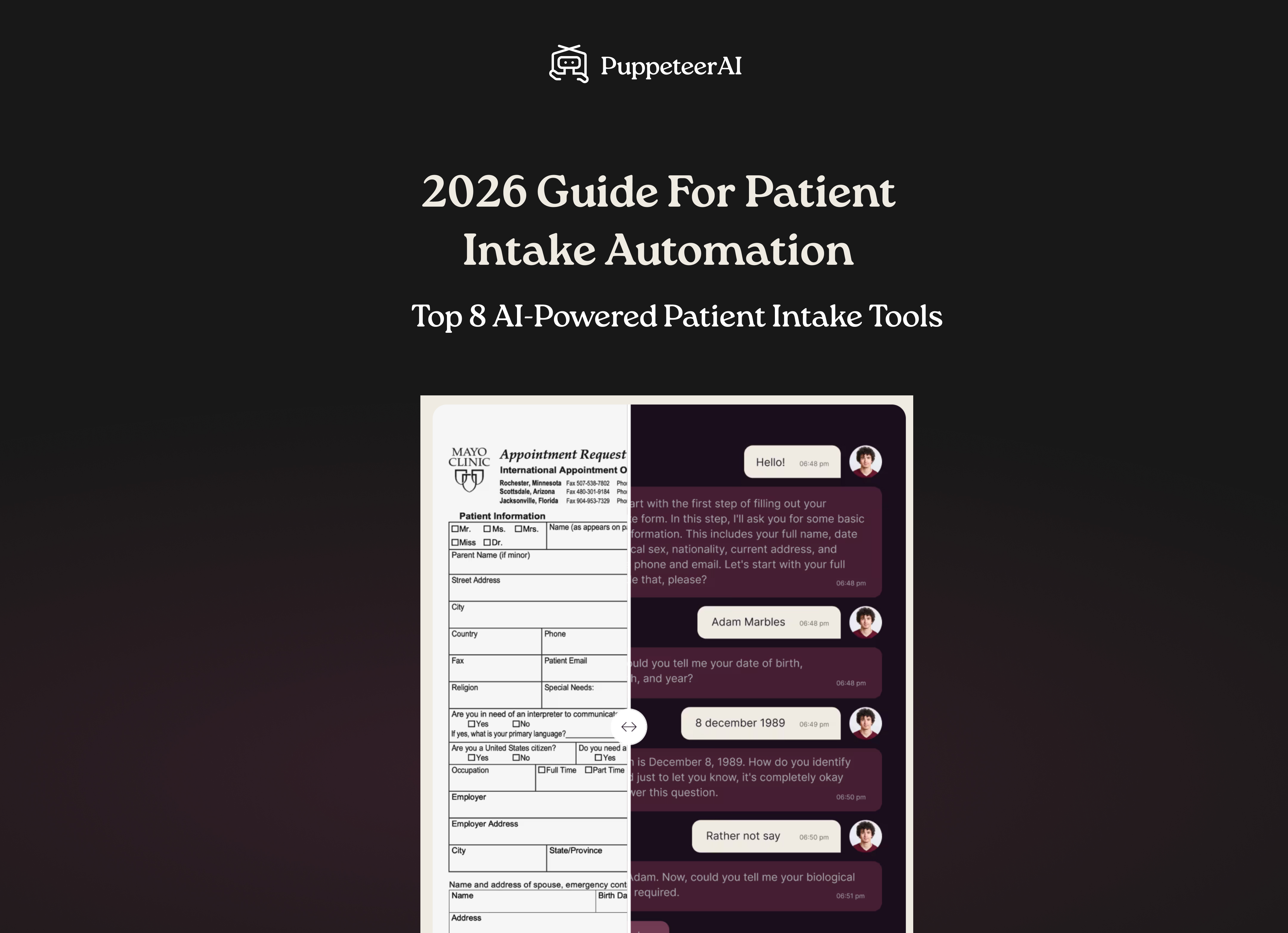
2026 Guide For Patient Intake Automation: Top 8 AI-Powered Patient Intake Tools
The Ultimate Guide to Patient Intake Automation in 2026: From Digital Forms to AI Agents
TL;DR: The Future of Intake is Conversational
- The Clipboard is History: Manual data entry and archaic paper forms are costing healthcare providers an average of $25 per patient record in administrative overhead.
- From Forms to Agents: In 2026, static digital forms have been superseded by Agentic AI (like Puppeteer AI) that engages patients via natural voice and text, increasing completion rates to over 90%.
- Interoperability is a "Price of Entry": 92% of healthcare leaders now prioritize FHIR/API-first integration, ensuring intake data flows directly into EHRs like Epic, Cerner, and athenahealth without human intervention.
- Immediate ROI: Organizations leveraging AI-driven intake see a 30-50% surge in administrative productivity and a 22% reduction in claim denials due to cleaner front-end data.
Introduction: The Invisible Barrier to Clinical Excellence
For decades, the "patient experience" has been gate-kept by a clipboard and a 10-page packet of photocopied forms. Despite the digital revolution of the 2010s, many healthcare organizations in 2026 were still trapped in "Digital Silos", where information was collected via a PDF, manually typed into an EHR by a burnt-out administrator, and then corrected weeks later when a claim was denied.
The Administrative Crisis of 2026
The global healthcare staffing shortage has reached a tipping point. According to the Bureau of Labor Statistics, the demand for healthcare support occupations is growing significantly faster than the average for all occupations. This has led to a front-desk turnover rate that is at an all-time high, with "administrative burden" cited by the American Medical Association (AMA) as a top-three driver of physician and staff burnout.
When intake is broken, the entire care delivery chain suffers. Inaccurate insurance data leads to denials; missing clinical history leads to redundant testing; and long wait times lead to patient attrition. This guide explores how automation, specifically the shift from static forms to Conversational AI, is solving these systemic issues.
"If a tool does not make providers' jobs better and easier and does not improve our patients' experience and lives, then it needs to stay on a shelf."— Dr. Richard Zane, Chief Innovation Officer at UCHealth
Top 8 Patient Intake Automation Solutions
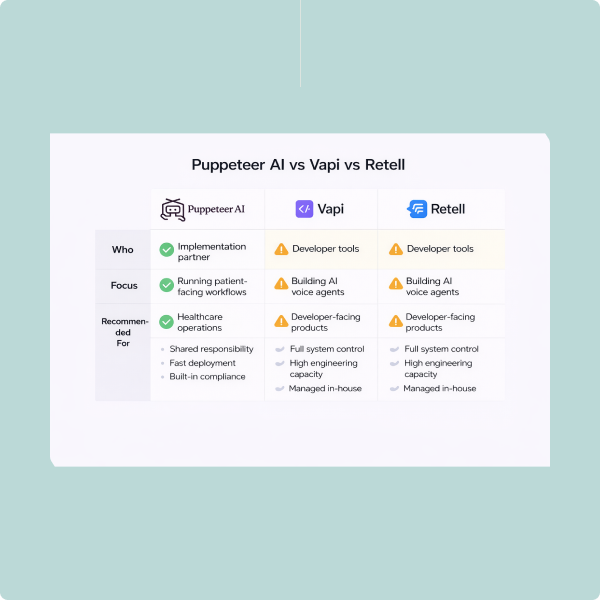
To help you evaluate the landscape fairly, we’ve standardized the top solutions across key metrics: Modality (how patients interact), Intelligence (ability to reason), Integration, Friction, and Primary ROI.
1. Puppeteer AI (The Conversational Leader)
Puppeteer AI represents the "3.0" of patient intake. While previous generations focused on moving paper forms to tablets, Puppeteer replaces the form entirely with an AI Agent.
- How it works: Instead of a link to a portal, patients receive a proactive call or text from an AI assistant. The agent engages in a natural conversation to gather demographics, medical history, and consent.
- Modality: Conversational AI (Natural Voice & Two-way Text).
- Clinical Intelligence: High. Puppeteer’s AI doesn’t just "collect" data; it validates it. If a patient mentions a medication that conflicts with their reason for visit, the AI can ask clarifying questions and flag it for the doctor.
- The Puppeteer Advantage: It meets patients where they are, on their phones, using their voices. It boasts the highest completion rate in the industry because it requires the least amount of "digital literacy."
- Primary ROI: Administrative labor replacement + 28% reduction in front-end denials.
2. Phreesia
A veteran in the space, Phreesia remains a powerhouse for large-scale health systems that require a "Digital Front Door" spanning multiple facilities.
- Modality: Digital Forms, Kiosks, and Mobile Web.
- Clinical Intelligence: Moderate. Uses branching logic for questionnaires.
- Integration: Deep, native integration with major EHRs.
- Patient Friction: Moderate. Requires navigating web portals or in-office hardware.
- Primary ROI: Point-of-service payment collection and standardization.
3. Luma Health
Luma focuses on "Patient Success Management," ensuring the journey from scheduling to intake is a single, continuous loop.
- Modality: SMS-based mobile web links.
- Unique Feature: Their "Actionable Reminders" allow patients to complete intake tasks directly within a text thread without logging into a separate portal.
- Primary ROI: Schedule density and "no-show" reduction.
4. Kyruus Health
Kyruus specializes in the "Search and Schedule" phase. By integrating intake directly into the provider search process, they ensure that by the time a patient books an appointment, much of their intake is already underway.
- Best For: Health systems focused on patient acquisition and "leakage" reduction.
- Intelligence: Low-to-Moderate (Process-driven).
5. Klara
Klara treats patient intake as a continuous conversation. It centralizes all communication (text, voice, and internal staff notes) into one collaborative dashboard.
- Modality: Secure Messaging/Chat.
- The Advantage: It feels like a messaging app, making it highly intuitive for younger, mobile-first demographics.
- Primary ROI: Enhanced patient-staff communication and improved NPS scores.
6. Notable
Notable uses "Intelligent Automation" (RPA + AI) to perform the manual tasks that staff used to do. It logs into the EHR and "types" the data into the fields, mimicking human behavior.
- Integration: RPA-driven (ideal for legacy EHRs that lack modern APIs).
- Primary ROI: Dramatic reduction in "manual click" time for administrative staff.
7. Yosi Health
Yosi provides an "app-less" experience, which is critical in an era of "app fatigue."
- Modality: Mobile Web Forms.
- The Highlight: Focuses heavily on the "waiting-room-less" experience, ensuring all data—including payments—is handled 24 hours prior to the visit.
8. Tebra (formerly Kareo + PatientPop)
For the independent, solo practitioner, Tebra offers a unified suite where the intake module is baked directly into their billing and EHR platform.
- Benefit: No "integration" needed because it is a single-database solution.
- Best For: Small, independent clinics.
Comparison Matrix: The 2026 Intake Landscape
FeaturePuppeteer AIPhreesiaNotableKlaraPrimary ModalityConversational (Voice/Text)Digital Forms / KiosksBack-office RPASecure MessagingUser IntelligenceHigh (Generative AI)Moderate (Logic Trees)Moderate (Task Bots)Low (Human-driven)Patient EffortLowest (Talking)Moderate (Typing/Login)Low (Invisible)Low (Texting)Data QualityAI-ValidatedUser-DependentHigh (Data Scraping)User-DependentSetup Speed2-4 Weeks8-12 Weeks12+ Weeks2-4 Weeks
Real-World Use Cases: Before & After
Scenario A: The Multi-Specialty Surgery Center
- Before: Staff spent 4 hours a day calling patients to confirm pre-op instructions and insurance. 15% of surgeries were delayed due to missing paperwork.
- After (with Puppeteer AI): AI Agents handle 100% of pre-op calls. The AI confirms the patient has fasted and identifies insurance discrepancies 48 hours in advance.
- The Result: 0% delays due to paperwork; 25% increase in surgical throughput.
Scenario B: The Mental Health Multi-Site Practice
- Before: Patients were asked to fill out sensitive PHQ-9 forms in a public waiting room on a clipboard. Disclosure rates were low due to privacy concerns.
- After (Conversational AI): Patients complete their assessments via a private, empathetic voice or text conversation in the comfort of their home.
- The Result: 32% higher reporting of critical symptoms, allowing for more accurate triage and better patient outcomes.
Scenario C: The High-Volume Urgent Care
- Before: Patients stood in line for 15 minutes to fill out clipboards. 12% of insurance cards were typed incorrectly, leading to significant uncollectible revenue.
- After (Automated Verification): A "Text-to-Check-in" agent handles all demographics and insurance verification via API while the patient is still in their car.
- The Result: Check-in time dropped to 45 seconds; denial rates dropped by 28%.
The 2026 Implementation Framework: The 4-Week "No-Paper" Plan
Transitioning to automated intake is no longer a multi-year project. With modern cloud architectures and AI, you can move from "Clipboards to Cloud" in a single month.
Week 1: The Friction Audit & EHR Mapping
Track a single patient's data journey. How many times do they provide their name? How many people touch that data before it hits the EHR? Identify the "bottlenecks." Simultaneously, map your EHR’s FHIR API capabilities.
- Requirement: Ensure your chosen tool has bidirectional sync (the ability to both read and write to the chart).
Week 2: AI Agent & Logic Design
This is where you design the "voice" of your practice. If using Puppeteer AI, you’ll configure the AI’s persona.
- Specialty Logic: For an Orthopedic clinic, the AI should be programmed to ask about imaging discs. For a Cardiology clinic, it should prioritize recent EKG locations.
- Escalation Triggers: Define when the AI should "hand off" to a human. (e.g., "If the patient reports chest pain, immediately bridge the call to the triage nurse.")
Week 3: Integration & Security Validation
Connect the AI Agent to your telephony and SMS systems. Execute the Business Associate Agreement (BAA) and perform a security audit. In 2026, Zero-Retention Architectures are the gold standard for PHI security.
Week 4: The "Silent Launch" & Scale
Run the AI for 10% of your appointments. Monitor the "Data Accuracy Rate." Once the AI reaches a 98% accuracy threshold on automated insurance verification, scale to 100% of the patient volume.
FAQ Section: Navigating the New Era of Automation
Q: How does Puppeteer AI differ from a basic chatbot?
A: A chatbot follows a rigid "If/Then" tree. Puppeteer is Agentic. It understands intent. If a patient goes off-script to ask, "Is there parking at the clinic?", the AI answers the question using the clinic's knowledge base and then seamlessly steers the conversation back to their medical history.
Q: Will elderly patients really use an AI voice agent?
A: Yes. Research from Gartner's Healthcare AI trends indicates that seniors find voice-based assistants more accessible than small-text mobile forms or complicated portals.
Q: How long does the ROI take to realize?
A: Most practices see a "break-even" within 90 days. The ROI comes from three streams: reduced labor hours, fewer claim denials due to clean data, and increased patient throughput (seeing more patients per day).
Q: Does the AI actually write to my EHR, or just send a summary?
A: Puppeteer AI writes structured data. This means the patient's "Birth Date" or "Allergies" go into the specific digital fields in Epic or athenahealth, rather than just appearing as a text note. This is the key to true automation.
Q: Can it handle multiple languages?
A: Yes. In 2026, AI agents can support over 50 languages with native-level fluency. A patient can start the conversation in English and switch to Spanish or Mandarin mid-sentence; the AI will adapt instantly and still record the results in English for the provider.
Conclusion: The Mandate for Change
The "Ultimate Guide" to patient intake is no longer a list of features; it is a blueprint for organizational survival. As we move through 2026, the practices that continue to rely on manual entry will be priced out of the market by "Smart Clinics" that leverage agentic intelligence to handle the "administrative tax" of healthcare.
By adopting tools like Puppeteer AI, providers can finally remove the wall of paperwork that stands between them and their patients, allowing doctors to be doctors and patients to feel seen, heard, and valued from the very first interaction.
Let’s build your next care agent together
Get a 20-minute call with our team to explore how Puppeteer AI can support your clinical workflows with custom AI agents.



Last Articles
Real Usecases, Real Results
See how healthcare teams use Puppeteer AI to automate patient conversations, reduce workload, and deliver better care, from intake to reactivation.